Healthy greetings Friends of TVD,
“Public Service Announcement”.
Two things, important to many in our TVD community. The first are two announcements from the hard working team at NARAL Pro-Choice America, commonly known as simply NARAL, whose 2.5 million members fight for reproductive freedom for everybody, including access to abortion care, birth control, paid parental leave, and protections from pregnancy discrimination. As you might imagine, this election year, their fight could not be bigger. Consider learning more, or joining them, at two upcoming virtual events: 1) Virtual salon series with their fearless leader Ilyse Hogue, on her new book The Lie That Binds. Tuesday 9/1, or Thursday 9/3 from 5:30 – 6:30 pm PST. RSVP using this Google form. And 2) Attend NARAL’s first ever Coast to Coast Virtual Luncheon on Wednesday, 10/7 from 12:30 – 1:30 pm PST. Attendees will have the opportunity to hear about the 2020 election landscape and the role NARAL will play in one of the most important election cycles of our lifetimes. You can register online here. Second, this upcoming Labor Day weekend is the (virtual) Kings Mountain Art Fair! Was there ever a better moment to support our volunteer firefighters up the hill on Kings Mountain by visiting (virtually) the King’s Mountain Art Fair? Not to mention the Elementary School! You can learn more here, or register for this year’s virtual event here.



NOTE: CV🦠News is a labor of love. If you enjoy reading this, please share widely! Was this forwarded to you by a friend? Please subscribe here.

IS THE SIX FOOT (TWO METER) RULE OUT OF DATE? NEW THOUGHTS ON PHYSICAL DISTANCING.
Since the beginning of the Coronavirus pandemic, the 6-foot rule has been used as a guide to keep us safe, along with washing our hands and wearing masks. We know that the latter two will help prevent the spread of COVID-19, but a new study calls this “safe distance” to avoid spread into question. The CDC recommends the 6-foot buffer based on past studies of infection among healthcare workers for diseases known to be spread by respiratory droplets, such as influenza, as coronavirus is thought to primarily be spread in the same way. The WHO actually recommends even less — staying just 3 feet away from anyone who is coughing or sneezing, but after the SARS-CoV-2 breakout, the 6-foot distance became the standard guideline in the US. However, as early as March 26, there were studies suggesting that Coronavirus particles can actually travel up to 23-27 feet.
The new paper that was released just last week in the British Medical Journal finds that the 2-meter (6-foot) safe physical-distancing rule is “an oversimplification’ based on outdated science of past viruses.” Part of the trouble is that respiratory droplets are usually just categorized as large or small in studies, but in reality, the sizes are on a continuum, so it’s not simple to determine if they will travel far or evaporate and land within 3-6 feet. The other very important factor is air flow around the droplets. Thus they proposed a more nuanced model which assumes that everyone is asymptomatic or presymptomatic and assesses the risk of viral transmission as it relates to “the four Cs: close, closed, crowded, continuous.” Based on the four Cs, you can determine risk and thus should extend the distance beyond 6 feet if the risk is medium or high. The chart really explains the results best:
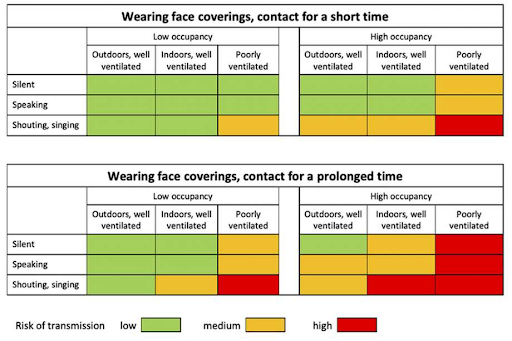
To simplify, if you or your loved ones have risk factors, it is safest to avoid any RED “high risk” situations and probably best to keep further distance than 6 feet in any YELLOW “medium risk” situations. That said, most importantly note that there is not a “no risk” classification here. You can make choices to limit your risk, but you cannot easily eliminate it if you are around others. Be safe, wash your hands, wear a mask, and keep your distance…maybe a bit more than 6 feet!
ARE THERE COVID LESSONS TO LEARN FROM THE POLIO OUTBREAKS OF THE 1950’S?
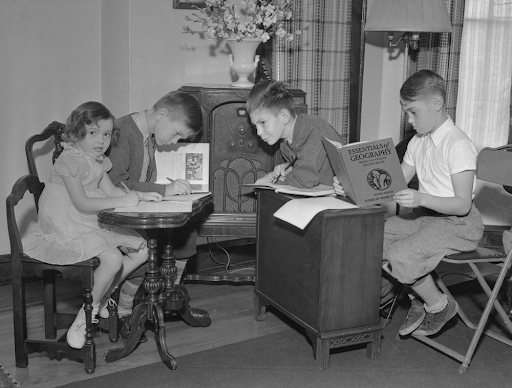
With so many photos over the last few weeks of smiling children in pajamas holding “My First Day of School” signs from their front door or living rooms, we have another set of memories for the COVID-19 time capsule – Fall 2020, when county by county, state by state, many schools chose not to reopen, and some did. While a recent Gallup poll shows a majority of parents don’t want their children back in classrooms full-time yet, the contortions in each home to facilitate remote learning for each child are tremendous and concerns that marginalized groups fall further behind are mounting. We find ourselves in complicated times.
A recent Time magazine article drew some interesting comparisons between the situation faced by parents today and that faced by parents during the polio outbreaks of the 1950’s. Polio struck communities seemingly at random. The United States had previously experienced outbreaks, but from the mid-1940s to mid-1950s, they came with relentless regularity. While the two diseases diverge significantly, the sense of powerlessness and unpredictability polio brought resonates in today’s COVID-19 pandemic, not least in the way outbreaks can affect the classroom. To read more, see Parents are facing tough choices about school in the COVID-19 Era. Here’s how people made the same decisions when it came to polio. Some highlights here:
- Mostly a summer illness, Polio often cropped up in the spring or lingered into fall, infringing upon the academic year—in San Antonio, Texas, an outbreak in the spring of 1946 closed schools at first for a couple of weeks and then for the remainder of the term, disrupting graduation festivities and prompting quarantines.
- Despite misunderstandings about how the virus was transmitted (mosquitoes and flies were incorrectly considered culprits), parents knew it was highly contagious, and spread when their children were in close contact with others. Social distancing—in the parlance of this pandemic—was the foremost countermeasure, even if it meant keeping kids cooped up when an outbreak abruptly halted summer fun.
- There was tremendous fear. Parents would give a “polio test” to their children every couple of days – can they touch their toes? Put their chin to their chest?
- It was a sickness harbored by silent carriers—the majority were asymptomatic, which scared parents. “Everything became a threat.”
- During the 1916 outbreak, New York City—which bore the brunt of the nation’s cases and deaths that year—shuttered schools based on rudimentary knowledge of how polio spread. When schools reopened and officials announced a policy of “leniency,” so many children were absent when classes resumed that there would often be only 2 or 3 children in a class of 30. In Minneapolis, a parents’ group lobbied successfully in favor of “playing safe” with additional delays, citing an enduring dilemma: “No one is absolutely sure of being right, one way or the other.”
- School closures elicited mixed reactions, with experts often disagreeing. Decisions were inherently unprovable because cases naturally fell when summer ended. Responses varied between localities, ranging from precautionary closures after one case to re-opening while polio lingered. The optimal level of acceptable risk was, as it is now, difficult to measure.
- When polio shut Chicago schools in 1937 during the Great Depression, it paralleled today’s concern that interruptions in learning could be devastating to students, and particularly those who were already the most disadvantaged. When educators experimented with radio lessons, the shift to at-home education magnified socioeconomic gaps—including disparities in access to technology.
The article concludes, “Polio was eventually defeated in the United States, thanks to vaccines administered to millions of schoolchildren in 1955. But the long journey to that point is a cautionary counterbalance to our impatience for a silver bullet to diminish the threat from COVID.” It goes on to state, “Perhaps the starkest truth the history of polio shows us is how little control we have in the face of a virus. Year after year, parents bore the anxiety of coping with an invisible threat to their children’s health, mitigating it as best they could within the constraints of their knowledge and foresight.”
Today, we look forward to a vaccine with cautious optimism, and stand in solidarity with all of the parents of today juggling work and their children’s remote learning, making decisions with limited information, and trying to do their best during challenging times.

DID THE CDC ADMIT THAT ONLY 6% OF COVID-19 DEATHS ACTUALLY DIED OF COVID-19? NO!
The phrase “only 6%” trended on Twitter over the weekend after a series of posts accused the US Centers for Disease Control and Prevention of quietly reducing the number of deaths due to COVID-19 from nearly 154,000 to a little more than 9,200, or 6 percent of that initial total.
Several of the posts, which were widely shared across social media networks before being taken down for violating platform policies, were later linked to followers of the QAnon conspiracy group. This organization has been known to spread false news in the past. President Donald Trump retweeted at least two of the statements only to fuel the fire of this incorrect statement.
In fact, the CDC did not “quietly say” that only 6% of the reported COVID-19 deaths were actually due to the virus. What it does say is the 6% of the 154,000 deaths reported since March COVID-19 is the sole cause of death listed on a death certificate. This means that 94% of those deaths were in people who had other contributing conditions listed such as diabetes, high blood pressure, asthma and cancer. Lots of people have one or two chronic medical conditions.
The CDC’s website provides weekly updates and the agency includes information on additional conditions present in patients who died with COVID-19. These other illnesses or conditions found to be present in a patient are called comorbidities. The agency also includes a chart detailing the number of patients with each additional condition.
This latest twisting of data reminds we need to be cautious in interpreting statistics and that there are groups who intentionally misrepresent the facts.

If you have made it this far, time for a reward, something to lighten your day, and acknowledge the human spirit. Find some escape, or perhaps even inspiration, in this ever growing collection of works and perspectives gathered from around the world. Please contact me directly if you have come across something that has lifted your heart today. Dr. Eric Weiss

Friends in Jaipur, India, have made sets of cotton face masks from delightful Indian prints. They would like to sell them in sets of 10, one of each design, the cost would be $50 ($5 each). These funds will be donated to the Shared Wisdom non-profit fund, which is dedicated to supporting individuals and communities as they offer their teachings and wisdom into the public domain. Funds will be shared with local social outreach programs as well as in support of spiritual endeavors throughout the world. Your donation will be tax deductible for $3 for each mask. Written receipts will be emailed to you by year end. If you would like to purchase a set, please email [email protected]
Speaking of masks…your and my best friend, “Uncle Rob”, asks the question, “Covid-19 vs Surgical Mask. Do Masks Work Or Not?”. Oh, boy. Let’s just say that his tagline is “fill it with gasoline”… Enjoy (and don’t try this at home)!
Again, CV🦠News is a labor of love. If you enjoy reading this, please share widely! Was this forwarded to you by a friend? Please subscribe here.
*****
Yours, in health and resilience,
Eric and the TVD MD team…