Digital greetings, Friends of TVD!
Here is the sixth issue of CV🦠News. It is remarkable to me how quickly time, even “pandemic time,” is passing. Again, thank you to all five of our physicians, and also the various contributors to our Hope and Grace page, a collection of works and perspectives gathered from around the world. If you’d like to receive this weekly newsletter in your inbox, please sign up here.
(CAUTIOUS) PROGRESS: EARLY PHASE TWO IN SAN MATEO
On May 13, 2020, San Mateo County’s Health Officer Dr. Scott Morrow said he intends to issue a new shelter in place order, effective on May 18, that would bring San Mateo County in line with the early Phase 2 guidelines of the governor’s Resilience Roadmap. The Roadmap allows for curbside and delivery activities for retail. Logistics and manufacturing, along with some other businesses, can open with modifications. Dr. Morrow expects to release the local health order, in line with the state order, later this week.
Dr. Morrow says “I am encouraged that data about COVID-19 cases, hospital capacity, and other indicators show some stability so that San Mateo County can now enter the early stages of Phase 2. I want to remind everyone these modifications are not being made because it is safe to be out and about. The virus continues to circulate in our community, and this increase in interactions among people is likely to spread the virus at a higher rate. Whether these modifications allow the virus to spread out of control, as we saw in February and March and resulted in the first shelter in place order, is yet to be seen. The social distancing and face covering directives, along with the prohibition on gathering, will remain in place since the risk of exposure to COVID-19 looms large for all of us. The public and open businesses need to fully do their part to minimize transmission of the virus.”

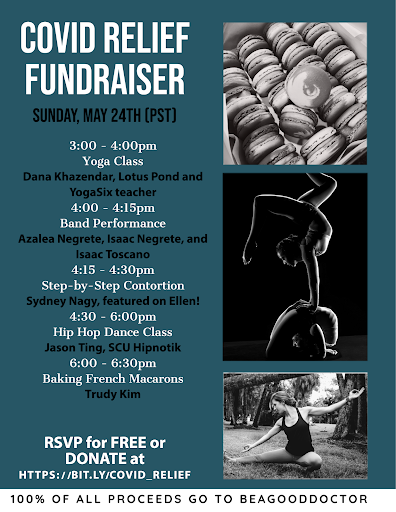
GIVING BACK?
There are many ways to give to our community these days, and our community, and the world at large, hasn’t seen such challenging times for a generation. Let me bring your attention to a cause which is near and dear to our healthy hearts, the non-profit “Be A Good Doctor,” founded by our very own Dr. Jennifer Abrams (back at Stanford when she was neither Abrams nor yet a Doctor). Full disclosure, yours truly is also on its Advisory Board. BeAGoodDoctor is fundraising to support efforts in the Emergency Department (ED) at Santa Clara Valley, a county hospital at the front lines of the local COVID pandemic. Our volunteer interpreters are fundraising for iPads to provide necessary virtual interpretation services in the ED and we’re training a new cohort to cover all of the unmet interpretation needs in the ED (nights and weekends when hired interpreters are not available). We are hosting a COVID relief fundraiser featuring fun Zoom activities throughout the day on Sunday, May 24th, featuring a yoga class with a teacher at YogaSix and Lotus Pond, a band performance, hip hop dance class, french macaron baking and step-by-step contortion done by a performer who was featured on Ellen! RSVP for free and donations can be made to BeAGoodDoctor here!

CDC UPDATES: “TEST BASED STRATEGY”
How long do you need to isolate if you feel sick and are concerned you have COVID, but couldn’t get tested?
The CDC’s recommendations have been updated as recently as May 3rd to reflect evolving information on persistent viral shedding after infection and to further delineate two approaches: a ‘symptom-based strategy’ and a ‘test-based strategy’ for discontinuation of home isolation. In the May 3rd updates, the home isolation period for the ‘symptom-based strategy’ was increased from 7 to 10 days since symptoms first appeared and the FDA states they will continue to revise as additional evidence becomes available. Because persistent viral shedding has been shown to last for several weeks after first appearance of symptoms in some patients, to be safest we have been recommending a slightly longer period of home isolation, a full 14 days since first symptoms appeared. In addition to the time since first symptoms, the CDC also specifies you should have had no fever for at least 72 hours (without the use of fever reducing medications) and that other symptoms (i.e. cough, shortness of breath) should have improved. A patient can opt for repeat testing once they no longer have a fever for 3 days and other symptoms have improved. This ‘test-based’ strategy for discontinuing home isolation requires two negative tests in a row at least 24 hours apart. The CDC has also updated their recommendations for patients who did not have symptoms but had a positive test (e.g. those with a positive contact who were then tested themselves despite being asymptomatic) – for these patients, home isolation is recommended until 10 days have passed since the first positive test and they continue to be symptom-free since the test (symptom-based strategy), or until they have two negative tests in a row at least 24 hours apart (test-based strategy).

CAN UV LIGHT KILL THE CORONAVIRUS?
There have not been conclusive studies done to show whether or not UV light can kill coronavirus specifically, but based on evidence that it kills bacteria, fungi and viruses (including the flu,) presumably it is effective against coronavirus as well. The same team at Columbia that studied the flu has shown that UV light can eradicate two types of airborne seasonal coronaviruses and they are now testing SARS-CoV-2, so better data should be available soon. The high frequency of UV light kills microbes by damaging the DNA or RNA code and triggers mutations that prevent the micro-organisms from reproducing. The UV light in germicidal fixtures is not the sunburn-causing UVA and UVB light, but rather UVC light, which has shorter wavelengths than the others. Far-UVC light cannot reach or damage living human cells and is thus the technology being investigated for use in public spaces. Currently, conventional germicidal UV lights are being used to sterilize unoccupied hospital rooms and subway cars, but there are other smaller permanent and portable devices that are potentially useful as well. You may have seen blue lights high on the wall in restaurants and airports before; these lights use technology called “upper-room ultraviolet germicidal irradiation” and there is hope that they could play a role in containing further spread of coronavirus if they can truly “zap pathogens out of the air in stores, restaurants and classrooms.” Various studies have shown UV light fixtures to be effective in disinfecting air in relatively small areas with good ventilation, so one of the challenges will be investigating the effectiveness in different settings. Dr. Srebric, a professor of mechanical engineering who is studying UV light said “I know it will definitely improve safety, but I cannot tell you by how much or how safe or whether I would go to a mall.” Amazon has built a robot that would be able to roll down the aisles in stores and warehouses to hopefully kill the virus on surfaces. There are also handheld devices such as those that sterilize cell phones and small personal items or wands that could be used to sterilize larger surfaces. Most of these products claim to kill 99.9% of bacteria and viruses, so odds are relatively good that coronavirus will also fall victim to UVC light. If you plan to use any of the consumer devices, please remember to follow the directions closely and never look at the light or use it directly on your skin and remember that hand-washing and other preventative measures should be continued as well. Read more (our sources) on UV light and COVID at The New York Times and New York Magazine.

DISPATCH #7: TIME FOR OFFENSE, NOT DEFENSE
“American exceptionalism is being challenged. Right now. We’ll figure out how to optimize physical distancing and we’ll eventually get the right cocktail of treatments, yet our current state of affairs is all defense. For the first time in US history, all 50 states have declared states of emergency.” Although published last month, this essay by my friend and colleague, Dr. Jordan Shlain, is compelling and information rich. I strongly recommend that you read it here.
IT HAS BEEN AWHILE, IS THERE A GOOD REVIEW ARTICLE TO RECOMMEND?
Yes! We agree, as this pandemic continues on, it is easy to be overwhelmed, and even confused, by the amount of information coming at us every day. Of course, part of the goal of our “CV🦠News” newsletter is to filter and parse your mental inbox. However, on April 29th, The Atlantic published a really excellent review of the Virus, the Disease, the Research, the Experts, the Messaging, the Information, the Numbers, and lastly, the Narrative. I recommend that you read the full article here. However, here is a bit of a summary to get you started (thank you again Ed Yong and his team at The Atlantic for this piece):
Much about the pandemic is maddeningly unclear. Why do some people get really sick, but others do not? Are the models too optimistic or too pessimistic? Exactly how transmissible and deadly is the virus? How many people have actually been infected? How long must social restrictions go on for? Why are so many questions still unanswered? The confusion partly arises from the pandemic’s scale and pace.
There isn’t just one coronavirus. Besides SARS-CoV-2, six others are known to infect humans—four are mild and common, causing a third of colds, while two are rare but severe, causing MERS and the original SARS. But scientists have also identified about 500 other coronaviruses among China’s many bat species.
SARS-CoV-2 is the virus. COVID-19 is the disease that it causes. The two aren’t the same. The disease arises from a combination of the virus and the person it infects, and the society that person belongs to. Some people who become infected never show any symptoms; others become so ill that they need ventilators. The virus might vary little around the world, but the disease varies a lot. This explains why some of the most important stats about the coronavirus have been hard to pin down. Estimates of its case-fatality rate (CFR)—the proportion of diagnosed people who die—have ranged from 0.1 to 15 percent. It’s frustrating to not have a firm number, but also unrealistic to expect one.
The CFR’s denominator—total cases—depends on how thoroughly a country tests its population. Its numerator—total deaths—depends on the spread of ages within that population, the prevalence of preexisting illnesses, how far people live from hospitals, and how well staffed or well equipped those hospitals are.
Human beings are notorious for our desire to see patterns,” says Vinay Prasad, a hematologist and an oncologist at Oregon Health and Science University. “Put that in a situation of fear, uncertainty, and hype, and it’s not surprising that there’s almost a folk medicine emerging.”
“Clinicians are under tremendous stress, which affects our ability to process information,” says Zoë McLaren, a health-policy professor at the University of Maryland at Baltimore County. “‘Is this actually working, or does it seem to be working because I want it to work and I feel powerless?’”
Since the pandemic began, scientists have published more than 7,500 papers on COVID-19. But despite this deluge, “we haven’t seen a lot of huge plot twists,” says Carl Bergstrom, an epidemiologist and a sociologist of science at the University of Washington. This is how science actually works. It’s less the parade of decisive blockbuster discoveries that the press often portrays, and more a slow, erratic stumble toward ever less uncertainty. That said, the precise magnitude of the virus’s fatality rate is a matter of academic debate. The reality of what it can do to hospitals is not.
Related, the scientific discussion of the Santa Clara study might seem ferocious to an outsider, but it is fairly typical for academia. Yet such debates might once have played out over months. Now they are occurring over days—and in full public view. “People from partisan media outlets find this stuff and use a single study as a cudgel to beat the other side,” Bergstrom says. “The climate-change people are used to it, but we epidemiologists are not.”
Like many COVID-19 studies, the Santa Clara one was uploaded as a preprint—a paper that hasn’t yet run the peer-review gauntlet. Preprints also allow questionable work to directly enter public discourse. For example, the editor at the Journal of Virology, says that she and her colleagues have been flooded with submitted papers, most of which are so obviously poor that they haven’t even been sent out for review. “They shouldn’t be published anywhere,” she says, “and then they end up [on a preprint site].” Some people are genuinely trying to help, but there’s also a huge amount of opportunism.”
Expertise is not just about knowledge, but also about the capacity to spot errors. We hunger for information, but lack the know-how to evaluate it or the sources that provide it. In a pandemic, the strongest attractor of trust shouldn’t be confidence, but the recognition of one’s limits, the tendency to point at expertise beyond one’s own, and the willingness to work as part of a whole.
The instinct to be calm and measured is laudable—until it isn’t. If officials—and journalists—are clear about uncertainties from the start, the public can better hang new information onto an existing framework, and understand when shifting evidence leads to new policy. “We go seeking fresher and fresher information, and end up consuming unvetted misinformation that’s spreading rapidly,” Bergstrom says. Historically, people would have struggled to find enough information. Now people struggle because they’re finding too much.
It does not help that online information channels are heavily personalized and politicized, governed by algorithms that reward certain and extreme claims over correct but nuanced ones. On Twitter, false information spreads further than true information, and at six times the speed.
When looking at case counts, remember this: Those numbers do not show how many people have been infected on any given day. They reflect the number of tests that were done (which is still insufficient), the lag in reporting results from those tests (which can be long), and the proportion of tests that are incorrectly negative (which seems high).
COVID-19 deaths are counted based either on a positive diagnostic test for the coronavirus or on clinical judgment. Flu deaths are estimated through a model that looks at hospitalizations and death certificates, and accounts for the possibility that many deaths are due to flu but aren’t coded as such. If flu deaths were counted like COVID-19 deaths, the number would be substantially lower. This doesn’t mean we’re overestimating the flu. It does mean we are probably underestimating COVID-19.
And statistics are important. One antibody test claims to correctly identify people with those antibodies 93.8 percent of the time. By contrast, it identifies phantom antibodies in 4.4 percent of people who don’t have them. That false-positive rate sounds acceptably low. It’s not. Let’s assume 5 percent of the U.S. has been infected so far. Among 1,000 people, the test would correctly identify antibodies in 47 of the 50 people who had them. But it would also wrongly spot antibodies in 42 of the 950 people without them. The number of true positives and false positives would be almost equal. In this scenario, if you were told you had coronavirus antibodies, your odds of actually having them would be little better than a coin toss.
The numbers still matter; they’re just messy and hard to interpret, especially in the moment. “I think people underestimate how difficult it is to measure things,” Natalie Dean, a statistician at the University of Florida says. “For us who work in public health, measuring things is, like, 80 percent of the problem.”
If measuring the present is hard, predicting the future is even harder. “There are two lessons one can learn from an averted disaster,” Zeynep Tufekci, a sociologist at the University of North Carolina says. “One is: That was exaggerated. The other is: That was close.”
The coronavirus not only co-opts our cells, but exploits our cognitive biases. Humans construct stories to wrangle meaning from uncertainty and purpose from chaos. We crave simple narratives, but the pandemic offers none. The facile dichotomy between saving either lives or the economy belies the broad agreement between epidemiologists and economists that the U.S. shouldn’t reopen prematurely. The lionization of health-care workers and grocery-store employees ignores the risks they are being asked to shoulder and the protective equipment they aren’t being given.
And the desire to name an antagonist, be it the Chinese Communist Party or Donald Trump, disregards the many aspects of 21st-century life that made the pandemic possible: humanity’s relentless expansion into wild spaces; soaring levels of air travel; chronic underfunding of public health; a just-in-time economy that runs on fragile supply chains; health-care systems that yoke medical care to employment; social networks that rapidly spread misinformation; the devaluation of expertise; the marginalization of the elderly; and centuries of structural racism that impoverished the health of minorities and indigenous groups. It may be easier to believe that the coronavirus was deliberately unleashed than to accept the harsher truth that we built a world that was prone to it, but not ready for it.

HOPE AND GRACE
If you have made it this far, time for a reward, something to lighten your day, and acknowledge the human spirit. Find some escape, or perhaps even inspiration, in this collection of works and perspectives gathered from around the world. Please contact me directly if you have come across something that has lifted your heart today. Dr. Eric Weiss

Graduates! Congratulations to the Class of 2020. John Krasinski highlights SOME GOOD NEWS around the world (including weather from Ryan Reynolds) and sends the class of 2020 off with advice from Oprah Winfrey, Steven Spielberg, Malala Yousafzai, and Jon Stewart. And thank you Samuel L. Jackson for the SGN dramatic re-enactment!
 Enjoy The official music video of UNICEF Goodwill Ambassador Angélique Kidjo’s “Pata Pata”, a fresh take on Miriam Makeba’s 1967 hit song. Once called the “world’s most defiantly joyful song”, “Pata Pata” has been re-recorded by Kidjo to spread information about COVID-19, with a focus on hundreds of millions of people in remote communities around the world.
Enjoy The official music video of UNICEF Goodwill Ambassador Angélique Kidjo’s “Pata Pata”, a fresh take on Miriam Makeba’s 1967 hit song. Once called the “world’s most defiantly joyful song”, “Pata Pata” has been re-recorded by Kidjo to spread information about COVID-19, with a focus on hundreds of millions of people in remote communities around the world.

And in closing this week, please enjoy listening to this lovely piece by one of our Friends of TVD, titled appropriately enough, “Moments of Grace.” Read more about KC and her work at the Compassion Institute here. Thank you, again, KC!
*****
Yours, in health and resilience,
Eric and the TVD MD team…